- Home
- /
- Health Conditions
- /
- Bacterial Vaginosis Treatment
Bacterial Vaginosis
4.6/5 based on 28000+ reviews
How our doctors can help
See a doctor now
From $39
Request a certificate
From $14.90
Request a referral
From $39
Request a script
From $18.90

When to consult a doctor for bacterial vaginosis?
If symptoms persist or worsen
If you experience unusual vaginal discharge, odour, itching or discomfort that does not improve on its own or worsens over time, seek medical attention and get the right treatment for bacterial vaginosis.
If it is recurrent or causes discomfort
If the bacterial vaginosis symptoms keep coming back or cause discomfort, pain and interfere with your daily life, speak to a doctor to identify the underlying causes and provide long-term management.
If you have health risks or are pregnant
If BV develops during pregnancy, or if you have a weakened immune system or underlying conditions, consult a doctor promptly. Untreated BV in such cases can increase the risk of complications.
This guide does not replace professional care. Consult a doctor to manage your symptoms. In emergencies, call 000 or visit a hospital immediately. The content is research-backed & medically reviewed by Dr Vishnu Gopalan, Co-Founder & Chief Medical Officer at Hola.
Causes and symptoms of bacterial vaginosis
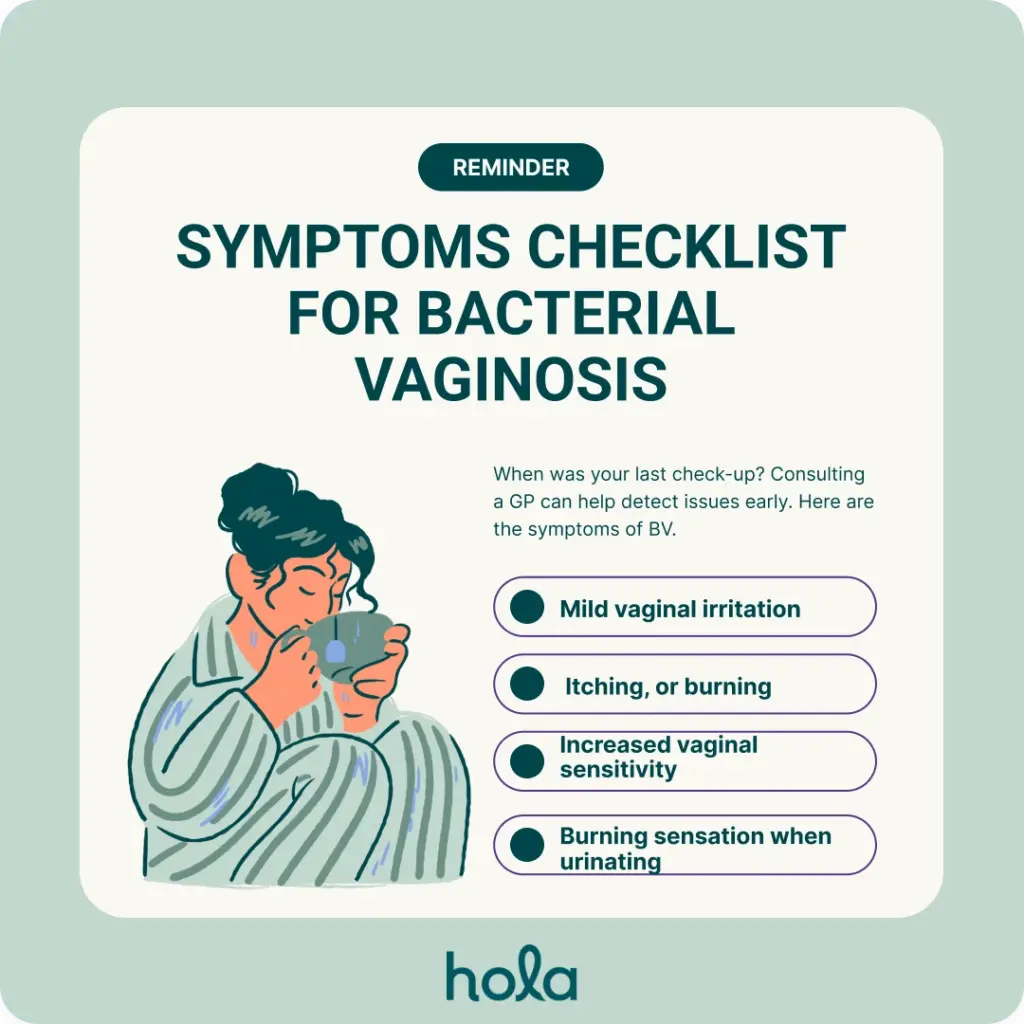
Bacterial vaginosis (BV) is often characterised by unusual vaginal discharge that typically has a strong fishy odour. Unlike other infections, it generally does not cause thick discharge. Common symptoms include mild vaginal irritation, itching, or burning, along with increased vaginal sensitivity. Some patients also experience a burning sensation when urinating. Bacterial vaginosis causes could be:
- Unprotected sex or having multiple sexual partners
- Douching
- Using scented soaps or vaginal washes
- IUDs or other contraceptive devices
- Smoking
- Recent use of antibiotics
Treatment and prevention of Bacterial vaginosis
The first step is to speak to a GP and complete the course of care or medication, if any. It is suggested to refrain from sex until recovered. Treat sexual partners if required. Avoid self-treatment. With a GP’s advice, some prevention methods for BV could include:
- Avoid touching or using scented vaginal products.
- Practice safe sex and use protection.
- Maintain good vaginal hygiene and stay dry.
- Wear breathable, cotton underwear.
- Avoid tight clothing for long periods.
- Limit multiple or new sexual partners.
Hola Health provides a fast and convenient way for you to see a doctor online in minutes, 24/7 across Australia. Much like an in-person GP clinic, our AHPRA-registered Australian telehealth doctor will conduct a comprehensive assessment to provide the best possible care, instantly.

Speak to our doctors 24/7
Providing consults for
Helpful resources
Download our Mobile App for better performance
- Book appointments instantly.
- Stay connected wherever you are.
- Experience healthcare, uninterrupted.
 Scan the QR Code to download the app instantly
Scan the QR Code to download the app instantly 

