Alzheimer’s progression: The 7 key stages explained
Written by the editorial staff writer at Hola. Medically Reviewed by Dr Nelson Lau, MBBS FRACGP, GP & Digital Health Specialist.
Contents
Summary: Alzheimer’s disease is a progressive brain disorder that gradually impairs memory, reasoning, and daily functioning. It develops in seven stages, beginning with no noticeable symptoms and eventually leading to profound mental and physical deterioration. Understanding these stages helps caregivers and families to identify changes, organise appropriate care, and provide necessary support. While there is no cure, timely diagnosis and effective treatment strategies can improve the quality of life for those affected by the condition.
Alzheimer’s disease is a progressive neurological disorder that gradually affects a person’s memory, thinking, behaviour, and ability to perform routine activities. It is the leading cause of dementia and becomes more common with advancing age. Understanding how Alzheimer’s progresses over time can help individuals, families, and caregivers better prepare for challenges ahead. Let’s examine the seven stages of Alzheimer’s disease to get a clear understanding of what to expect at each phase.
Briefly explain what Alzheimer’s disease is
Alzheimer’s disease is a progressive brain disorder that slowly impairs memory, thinking, and daily living skills. It is the most common cause of dementia and primarily affects older adults. It leads to problems with memory loss, confusion, and changes in behaviour. The condition gradually deteriorates, making it increasingly difficult for individuals to maintain their independence. While there is no cure, early diagnosis and care can help manage symptoms and enhance quality of life. Medical expert Dr Nelson Lau says that common early pathological changes (amyloid and tau accumulation) start 10-20 years before symptoms.Importance of understanding the stages—for patients, caregivers, and families
Understanding the stages of Alzheimer’s disease is crucial for patients, caregivers, and families, as it helps them anticipate what lies ahead as the illness progresses. For patients, it offers insight into the changes they may experience and encourages early planning. Caregivers can prepare for evolving care needs and adjust support accordingly, reducing stress and enhancing the quality of care. Families gain a better understanding of the challenges they may face, enabling them to offer more robust emotional support and to make informed decisions regarding medical care, housing, and safety precautions. Overall, this understanding fosters empathy, patience, and better management throughout the disease.Difference between Alzheimer’s and general dementia.
Dementia refers to a collection of symptoms that impact memory, cognitive function, and social skills to a degree that disrupts everyday life. It is not a distinct illness but rather a general term for various disorders affecting the brain. Alzheimer’s disease, in contrast, is the most prevalent form of dementia. It is a specific neurological condition that leads to gradual memory decline, confusion, issues with communication, and behavioural changes due to the accumulation of abnormal proteins and damage to neurons. In essence, Alzheimer’s is a type of dementia, but not every case of dementia is Alzheimer’s. Other variants include vascular dementia, Lewy body dementia, and frontotemporal dementia, each having unique causes and symptoms. Although treatment and care strategies may share similarities, accurate diagnosis is crucial for determining the most effective ways to manage symptoms and organise care.Ready for positive change? Start your mental health care plan here.
Book an appointment
Fully bulk-billed, across Australia.
Importance of identifying stages for care and treatment planning.
Identifying the various stages of a condition like Alzheimer’s is essential for effective treatment and care planning. Understanding the stage enables healthcare professionals to ensure that support is both suitable and timely. The early stages might emphasise preserving independence and providing memory assistance, while advanced stages necessitate more comprehensive care and safety precautions. Understanding these stages helps patients and their families establish realistic expectations about the progression of the disease, alleviating uncertainty and stress. It informs decisions about medications, lifestyle changes, and identifies when to pursue additional support or professional assistance. In summary, a clear understanding of stages enhances quality of life by facilitating personalised care plans, optimal resource distribution, and robust emotional support throughout the experience.How stages help manage expectations for both patients and families.
Comprehending the stages of a condition like Alzheimer’s allows both patients and their families to set realistic expectations. Awareness of anticipated changes at each phase diminishes anxiety and emotionally prepares everyone for future challenges. Patients are more capable of understanding their condition and actively participating in care planning, while families are better prepared to foresee the support needed and prevent feeling overwhelmed by sudden changes. This understanding encourages open dialogue, patience, and empathy, nurturing stronger connections. Ultimately, having a clear grasp of the stages enables families to prepare for the future, access resources promptly, and stay focused on preserving quality of life, thereby making the caregiving experience less overwhelming and more manageable.Stages of Alzheimer’s disease
Alzheimer’s disease progresses gradually over time, affecting memory, thinking, and behaviour. Understanding each stage helps caregivers and families prepare for changing needs. While there are seven Global Deterioration Scale (GDS) stages, most clinicians often collapse these into three practical stages (early, moderate, late) for care planning.Stage 1: No impairment
During this stage, individuals operate normally without any noticeable symptoms. Any initial signs may only be detectable through brain imaging or specialised assessments.Stage 2: Very mild decline
Minor memory lapses begin to occur, such as forgetting names or misplacing things. These changes often mimic typical aging and may go unnoticed by others. Neuropsychological testing can still be normal and longitudinal change is key.Stage 3: Mild cognitive decline
Memory and focus issues become more evident. Close friends or family might begin to notice subtle changes in communication or decision-making.Stage 4: Moderate cognitive decline
Symptoms become more noticeable. Individuals may find it challenging to manage bills, organise events, or remember recent discussions. Driving safety should be formally reviewed.Stage 5: Moderately severe decline
Assistance is required for daily activities such as dressing or preparing meals. Memory loss becomes increasingly pronounced, particularly concerning personal history.Stage 6: Severe decline
Individuals may need constant supervision. They might forget loved ones, become disoriented in their surroundings, and exhibit changes in personality or behaviour.Stage 7: Very severe decline
In this final stage, individuals may lose the ability to speak, walk, or control bodily movements. Full-time care becomes necessary, and planning for end-of-life care is crucial.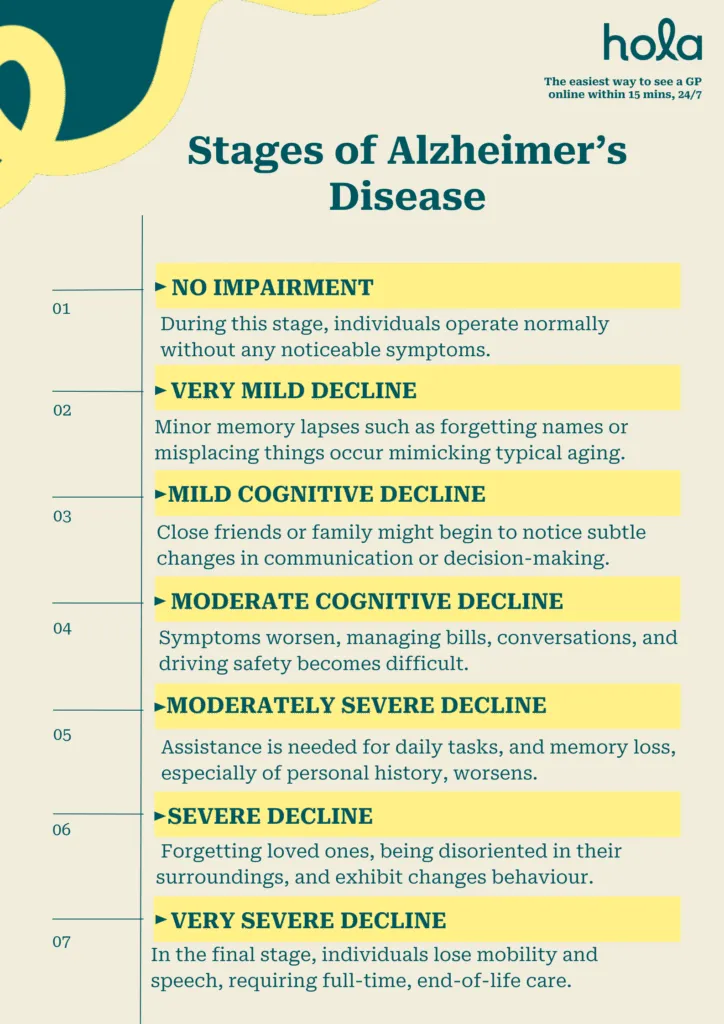
Living with Alzheimer’s: What to expect
Living with Alzheimer’s disease is a journey filled with emotional, physical, and practical challenges for both the individual and their family members. As the condition advances, memory loss and confusion may lead to frustration, personality changes, and increased dependence on others. Daily tasks that were once simple can become difficult or require assistance, and communication may become strained. Families often assume caregiving responsibilities, which can be both fulfilling and overwhelming. It is vital to create a safe, structured environment and to modify daily routines as needs change. Emotional support, patience, and proactive planning are essential for maintaining quality of life. Professional assistance, whether in-person or through telehealth, can help navigate changes, manage symptoms, and provide necessary support for caregivers. Although the disease introduces many challenges, understanding what to expect fosters better care, stronger relationships, and more moments of connection. Dementia Australia’s National Dementia Helpline (1800 100 500) provides 24-hour advice.How to support a loved one at each stage
Assisting a loved one with Alzheimer’s requires adapting your care as their needs evolve throughout the disease. In the early stages, promote their independence and provide memory aids such as calendars or reminders. Practice patience and listen, allowing them to share their feelings and concerns. During the middle stages, offer more direct assistance with daily activities like dressing, cooking, and medication prompts or Webster-packing. Simplify communication by using straightforward, gentle language and creating a calm, organised environment to minimise confusion. It’s crucial to be alert to mood fluctuations and seek professional help if necessary. In the later stages, prioritise comfort and safety. Help with all personal care tasks and maintain routines that offer familiarity. Use touch, music, or familiar scents to foster emotional connections. Throughout all stages, demonstrate love, patience, and understanding, and do not hesitate to seek help to prevent caregiver burnout.Signs that indicate it’s time to consult a doctor.
If you or someone you care about shows signs of memory loss that interfere with daily life, like forgetting important dates or asking the same questions, it's crucial to consult a doctor. Start with your online GP. Telehealth can triage concerns, but formal diagnosis needs and in-person assessment. Additionally, any significant confusion about time, place, or familiar people should prompt a medical evaluation. If there are abrupt changes in mood, personality, or behaviour, like heightened aggression, withdrawal, or anxiety, seeking professional guidance is advisable—especially if depression treatment, anxiety treatment, or antidepressants treatment may be appropriate. Struggling with daily tasks such as managing finances, preparing meals, or maintaining personal hygiene is another strong sign that it's important to seek advice from a healthcare professional. Early assessment can aid in diagnosing the underlying issue, initiating treatment sooner, and providing support and resources for effective symptom management, including obtaining a medical certificate for caregiving related to Alzheimer’s or a general medical certificate if needed.Conclusion:
Understanding the seven stages of Alzheimer’s disease helps families and caregivers to anticipate changes and offer appropriate assistance. While there’s no cure, early detection and proper care can significantly improve the quality of life of those affected by the condition.FAQs
What is Alzheimer's disease?
Alzheimer’s disease is a progressive brain disorder that leads to memory loss, confusion, and challenges with reasoning and everyday activities. It is the most common form of dementia and gradually worsens. While there is no definitive cure, available treatments can help alleviate symptoms and improve overall health.What's the difference between Alzheimer's and dementia?
Dementia is a general term for a group of symptoms that impact memory, cognitive function, and social skills, to the point where they disrupt everyday life. Various medical conditions or neurological disorders can cause it. Alzheimer’s disease is the most common form of dementia. It is a distinct neurological disorder that triggers dementia symptoms by progressively damaging and destroying brain cells. So, Alzheimer’s is a type of dementia, but not all dementia is Alzheimer’s.Is Alzheimer's disease genetic?
Yes, it can be, but not always. In rare cases of early-onset Alzheimer’s (before age 65), it may be triggered by inherited genetic mutations. If a parent carries one of these mutations, their child has a 50% chance of developing the disease.How can I prevent Alzheimer's?
While there is no definitive way to prevent Alzheimer’s disease, you can reduce the risk by maintaining a healthy lifestyle. This involves regular exercise, eating a balanced diet, keeping your brain active through lifelong learning and meaningful social connections, managing health conditions like diabetes and hypertension, ensuring adequate sleep, avoiding tobacco, and limiting alcohol consumption. These measures help protect cognitive function and may help delay or reduce the risk of Alzheimer’s disease. Dr Nelson Lau added that WHO 2023 dementia risk-reduction guidelines also recommend the use of hearing-aids for those patients with hearing loss, and also reducing air-pollution exposure.What are the early warning signs of Alzheimer’s?
Warning signs of Alzheimer’s disease include:- Memory loss that disrupts daily functioning
- Trouble planning or solving problems
- Difficulty completing familiar tasks
- Confusion about time or place
- Problems with speaking or writing
- Poor judgment or decision-making
- Changes in mood or personality
How is Alzheimer’s diagnosed?
Alzheimer’s is diagnosed through a combination of medical history, cognitive assessments, physical and neurological exams, and imaging techniques such as MRI or CT scans. Blood tests are often used to eliminate other possible causes. In some cases, advanced diagnostic tools can detect brain changes linked to Alzheimer’s. Early diagnosis is crucial for effective care and treatment.Can an online GP diagnose Alzheimer’s disease?
An online general practitioner (GP) can evaluate early signs of Alzheimer’s via telehealth and begin the assessment process. However, a comprehensive diagnosis requires in-person tests such as cognitive exams, brain scans, and blood tests. Amyloid-PET and CSF or plasma biomarkers are now available in certain Australian memory clinics. The GP can provide a referral to a specialist for further evaluation.Do I need a referral to see a dementia specialist?
Yes, in most cases, you do need a referral from a general practitioner (GP) to see a dementia specialist, such as a neurologist or psychiatrist. The GP will evaluate your symptoms and refer you to the appropriate specialist for further assessment and diagnosis.How does telehealth help in managing Alzheimer’s disease?
Telehealth helps manage Alzheimer’s by allowing frequent virtual consultations, remote connections with doctors and specialists, caregiver support, medication reviews, and coordinated care planning. It improves convenience and ensures consistent care, especially for individuals with mobility or travel challenges.Take control of your mental health. Begin your care plan now.
Book an appointment
Fully bulk-billed, across Australia.
What we treat
- Cough
- Nausea & vomiting
- Fever
- Hayfever
- Fatigue
- Sore throat
- Acne
- Hair loss
- Gout
- Eczema
- Rosacea
- Sunburn
- UTI
- Erectile dysfunction
- Contraception
- Morning sickness
- Morning after pill
- Prostate health
- Anxiety
- Depression
- Stress
- Grief & loss
- Antidepressants
- Premature ejaculation
- Asthma
- Blood pressure
- Blood thinners
- Diabetes
- Cholesterol
- Migraines & headaches
- Allergies
- Body ache
- Heartburn & reflux
- Sleep disorder
- Pain relief
- Gastro
Related Articles
What Is Online Therapy? Everything You Need To Know About e-Therapy
February 19, 2026Mental Health
...
Disclaimer
This blog is for general informational purposes only and does not indicate that Hola Health provides all treatments or preventive measures mentioned. It is not intended to be a substitute for professional medical advice. Always seek the guidance of your doctor or other qualified health professional with any questions you may have regarding your health or a medical condition. For emergencies please immediately contact 000. Any medical topics discussed are intended to educate, not to imply availability through Hola Health.
 Facebook
Facebook  X
X  Copy Link
Copy Link