Understanding Infertility
Written by Dr Santanu Baruah, Founder, Medical Director , Fertility Specialist & Gynaecologist MBBS, MRCOG, FRANZCOG, FRCOG, CGES

Contents

Causes of Infertility
Healthcare providers consider a couple infertile if they try but fail to get pregnant within one year. When the woman is older than 35, the amount of time trying to conceive drops to six months for an infertility diagnosis. In women over 40, immediate evaluation is warranted.What causes infertility?
Causes of infertility vary:- 1 in 3 infertile women have a problem with the female reproductive system
- 1 in 3 infertile men have a problem with the Male reproductive system
- 1 in 3 couples have a problem that affects both of them or an undetermined issue.
How common is infertility?
An estimated 1 in 6 women between the ages of 15 and 44 have trouble conceiving. Types of infertility include:- Primary: A woman who was never pregnant and who can’t conceive after one year of not using birth control
- Secondary: Secondary infertility occurs when a woman can’t get pregnant again after having at least one successful pregnancy. Secondary infertility is just as common as primary infertility.
1.1 Understanding female infertility
How does the female reproductive system work?
The female reproductive system provides several functions. The ovaries produce egg cells, called the ova or oocytes. The oocytes are then transported to the fallopian tube where fertilization by a sperm may occur. The fertilized egg ( embryo) then moves to the uterus, where the uterine lining has thickened in response to the normal hormones of the reproductive cycle. Once in the uterus, the fertilized egg can implant into the thickened uterine lining and continue to develop. If implantation does not take place, the uterine lining is shed as menstrual flow (period).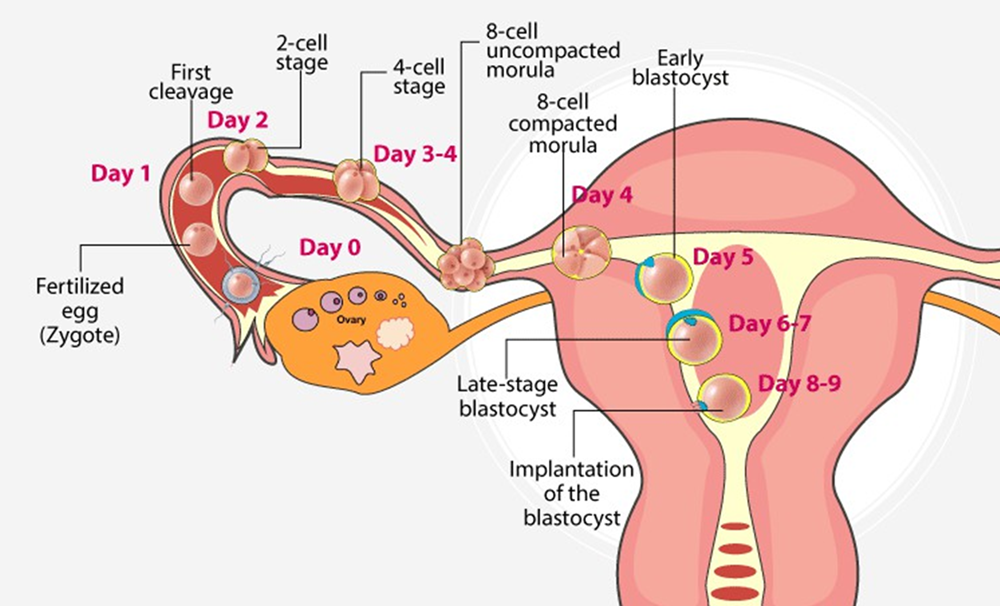 There are many possible causes of infertility. However, it can be difficult to pinpoint the exact cause, and some couples have “unexplained” infertility or “multifactorial” infertility (multiple causes, often both male and female factors). Some possible causes of female factor infertility can include:
There are many possible causes of infertility. However, it can be difficult to pinpoint the exact cause, and some couples have “unexplained” infertility or “multifactorial” infertility (multiple causes, often both male and female factors). Some possible causes of female factor infertility can include:
Cause of Infertility: |
Explanation: |
| Problems with the uterus | This includes polyps, fibroids, septum or adhesions inside the cavity of the uterus. Polyps and fibroids can form on their own at any time, whereas other abnormalities (like a septum) are present at birth. Adhesions can form after a surgery like a DCC. |
| Problems with the fallopian tubes | Tube blockage prevents the egg and sperm meeting in the fallopian tube and an embryo travelling into the uterus to implant. The most common cause of “tubal factor” infertility is pelvic inflammatory disease usually caused by chlamydia and gonorrhoea. |
| Problems with ovulation | There are many reasons why a woman may not ovulate (release an egg) regularly. Hormonal imbalances, thyroid problems, severe stress, substance abuse and pituitary issues are all examples of things that can affect ovulation. |
| Problems with egg number G quality | Women are born with all the eggs they will ever have, and this supply can “run out” early before menopause. In addition, some eggs will have the wrong number of chromosomes and cannot fertilize or grow into a healthy foetus. Some of these chromosomal issues (such as “balanced translocation”) may affect all of the eggs. Others are random but become more common as a woman gets older. |
Who is at risk for female infertility?
Many factors can increase a woman’s risk of female infertility. General health conditions, genetic (inherited) traits, lifestyle choices and age can all contribute to female infertility. Specific factors can include:- Age
- Hormone issue that prevents ovulation
- Being underweight and overweight
- Having a low body-fat content from extreme exercise
- Abnormal menstrual cycle
- Endometriosis
- Structural problems - such as fibroids, uterine septum
- Autoimmune disorders
- PCOS
- Sexually transmitted disease
- Excessive substance use (heavy drinking)
- Smoking
- A past history of ectopic pregnancy
Understanding Ovarian reserve
The term “ovarian reserve” refers to the number and quality of your eggs, also known as oocytes. If you have diminished ovarian reserve, this means that the number and quality of your eggs is lower than expected for your age.What is the average egg count by age?
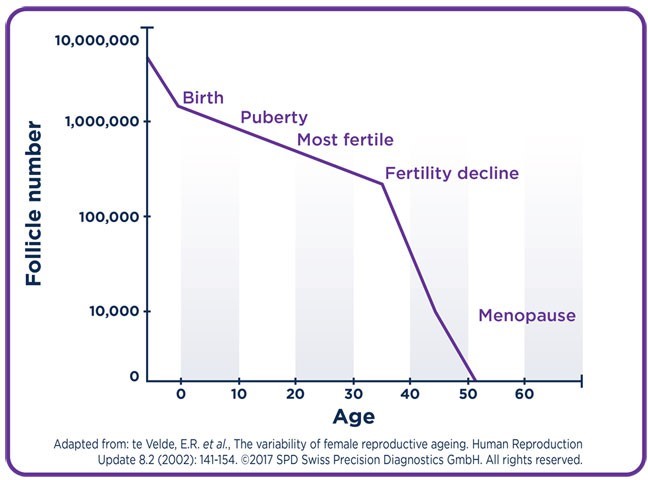
The “average” number of eggs in your ovarian reserve depends on age. Your own eggs were formed while you were still in utero. In other words, you’re born with all the eggs you’ll ever have. From there, your egg reserve decreases over time. During foetal life, there are about 6 million to 7 million eggs. From this time, no new eggs are produced. At birth, there are approximately 1 million eggs; and by the time of puberty, only about 300,000 remain. Of these, only 300 to 400 will be ovulated during a woman's reproductive lifetime. Fertility can drop as a woman ages due to decreasing number and quality of the remaining eggs. These are the average number of eggs you have at each age:| Age | Estimated No. of Eggs (Oocytes) |
| 20 weeks of gestation | 6 to 7 million |
| Birth | 1 to 2 million |
| Puberty | 300,000 to 500,000 |
| Around age 37 | Roughly 25,000 |
| Around age 51 – average age of menopause | Roughly 1,000 |
 While those with diminished ovarian reserve have fewer eggs than those without, there’s no clear consensus on the average number of eggs for those with the condition. Diminished ovarian reserve is generally defined by hormone levels and not by the number of eggs in the ovarian reserve, which makes the definition of the condition confusing. Since diminished ovarian reserve is diagnosed by blood tests measuring hormone levels, and not by counting eggs, it’s hard to determine the average number of eggs of someone who has the condition.
While those with diminished ovarian reserve have fewer eggs than those without, there’s no clear consensus on the average number of eggs for those with the condition. Diminished ovarian reserve is generally defined by hormone levels and not by the number of eggs in the ovarian reserve, which makes the definition of the condition confusing. Since diminished ovarian reserve is diagnosed by blood tests measuring hormone levels, and not by counting eggs, it’s hard to determine the average number of eggs of someone who has the condition.
Causes of diminished ovarian reserve
Aging naturally reduces your egg reserves. However, a number of other factors can cause diminished ovarian reserve. These include:- Tubal disease
- Endometriosis
- Prior ovarian surgery
- Chemotherapy
- Radiation therapy
- Smoking
- Pelvic infection
- Mumps
- Genetic abnormalities such as Fragile X Syndrome
- Autoimmune disease
Diagnosis of ovarian reserve
Ovarian reserve testing and female reproductive ageing:
- The evaluation of the ovarian reserve is carried out fundamentally by the determination of the serum Follicle Stimulating Hormone (FSH) and Estradiol (E2) levels early in the menstrual phase (basal state on days 1 to 4 of the cycle)
- and as well as the serum quantification of anti-Müllerian hormone (AMH) in the early follicular phase of the cycle.
- Counting of the ovarian antral follicles also represent one of the ways to assess ovarian reserve.
1.2 Understanding male infertility
Infertility is a common issue. Infertility affects one in every six couples who are trying to conceive. In at least half of all cases of infertility, a male factor is a major or contributing cause. This means that about 10% of all males in the Australia who are attempting to conceive suffer from infertility.Spermatogenesis – Production of sperm

What causes male infertility?
Many biological and environmental factors can impact your fertility. Possibilities include:
Cause of Infertility: |
Explanation: |
| Azoospermia | Your infertility can be related to your inability to produce sperm cells |
| Oligospermia | The production of low- or poor-quality sperm |
| Genetic diseases | Examples include Klinefelter’s syndrome, myotonic dystrophy, microdeletion and more |
| Malformed sperm | Sperm that cannot live long enough to fertilize the egg |
| Some medical conditions | Examples include Diabetes, some autoimmune disorders, cystic fibrosis and some infections |
| Some medications and supplements | |
| Varicocele | This is a condition where the veins on your testicles are larger than normal, causing them to overheat, which can affect the shape or number of your sperm |
| Cancer treatments | Chemotherapy, radiation or a surgery that removes the testicles (one or both) |
| Unhealthy habits | Heavy alcohol use, smoking, illegal drug use and anabolic steroids |
| Trauma to the testes | Injury |
| Hormonal disorders | Disorders that affect your hypothalamus or pituitary glands can affect your fertility |
Which males are more likely to have infertility?
Some males are more likely than others to experience infertility. You might be more likely if:- You’re overweight or obese
- You’re age 40 or older
- You’ve been exposed to radiation
- You’ve been exposed to environmental toxins including lead, calcium, pesticides or mercury
- You’re a tobacco, marijuana or alcohol abuser
- You’re taking some medications including cyproterone, flutamide, spironolactone, bicalutamide, cimetidine or ketoconazole
- You’re around heat that raises the temperature of your testes. Those who frequently use a sauna, hot tub or wheelchair might experience this
- You have a history of undescended testicle(s)
- You have a history of varicoceles, which are widened veins in the scrotum
- You’ve been exposed to testosterone. Some males need injections, implants or topical gel for low testosterone
| Semen Parameter | Reference Value |
| Volume | ≥ 1.5 ml |
| pH | 7.2 to 7.8 |
| Concentration | ≥ 15 x 106 / ml |
| Total spermatozoa (sperm) per ejaculate | ≥ 39 x 106 (≥ 39 million) |
| Progressive Motility | ≥ 32% motile |
| Total Motile | ≥ 40% (Progressive + Non Progressive) |
| Vitality | ≥ 58% live spermatozoa (sperm) |
| Normal Spermatozoa (Sperm) | ≥ 4% |
2. Investigation
It is important to carry out investigations on both partners. One third of infertility will be due to female factors, one third due to male factors and one third due to factors in both partners.2.1 Female testing
The following investigation is undertaken to determine possible causes of infertility and ensure good health in preparation for pregnancy.| TESTS | |
| CHEMISTRY | Fasting glucose, Fasting full lipid profile, HbA1c, Ferritin |
| INFECTIOUS DISEASES | Hepatitis B serology, Hepatitis C serology, HIV serology, Syphilis serology, Rubella serology, Chlamydia / Gonococcus PRC (urine) |
| HORMONES | Day 5 – 10 AMH, Prolactin, TSH (T4 if TSH is abnormal) Free testosterone, SHBG, DHEAS, Androstenedione, Day 3 – 17 hydroxyprogesterone |
| BLOOD | Blood group and antibodies, Full Blood Count (FBC), Screening for haemoglobinopathy where indicated |
| IMMUNOLOGICAL MARKERS | CA125 |
| ULTRASOUND | Pelvic ultrasound |
2.2 Male testing
The following investigation is undertaken to determine possible causes of infertility and ensure good health.| TESTS | |
| CHEMISTRY | Fasting glucose, Fasting full lipid profile, HbA1c |
| INFECTIOUS DISEASES | Hepatitis B serology, Hepatitis C serology, HIV serology, Syphilis serology, Chlamydia / Gonococcus PRC (urine) |
| HORMONES | Free testosterone, SHBG, DHEAS, Androstenedione |
| BLOOD | Blood group and antibodies, Full Blood Count (FBC), Screening for haemoglobinopathy where indicated |
| SEMEN | Semen analysis |
2.3 Genetic testing
Male infertility:
Genetic testing is indicated if there is a diagnosis of azoospermia or severe oligospermia as genetic conditions may be responsible for up to 15% of all cases. Currently, three genetic tests are commonly performed: karyotype analysis (KA), Y-chromosome microdeletion testing, and CFTR mutation testing. Despite widespread adoption of these tests, an aetiology for infertility remains elusive in up to 80% of cases.Female infertility:
Routine genetic testing is often recommended for female patients undergoing in vitro fertilization (IVF) to screen for certain genetic conditions and chromosomal abnormalities. This can include carrier testing for specific genetic diseases such as cystic fibrosis or sickle cell anaemia, as well as pre-implantation genetic testing (PGT) for aneuploidy, which is the presence of an abnormal number of chromosomes in an embryo. PGT can be performed on embryos created during an IVF cycle prior to transfer, to determine which embryos are most likely to result in a healthy pregnancy. Routine genetic testing can provide valuable information for both the patient and the healthcare provider, allowing for informed decisions about the best course of action for a successful pregnancy. However, it is important to note that not all patients may choose to undergo routine genetic testing and the decision ultimately depends on individual circumstances and preferences.3. Treatment Options
a. Ovulation induction:
Infertility is a challenging experience that can take a toll on a person's emotional and financial well-being. Our goal is to ease this burden by offering top-notch treatment combined with personalized care at an affordable cost. To achieve this, we have assembled a team of compassionate and knowledgeable doctors, embryologists, nurses, and staff who will be with our patients every step of the way. Our commitment is to provide comprehensive, end-to-end support to help make this journey as smooth as possible.b. Intra Uterine Insemination (IUI):
Intra uterine insemination or Assisted insemination: Intrauterine Insemination (IUI) is a fertility treatment that involves placing sperm directly inside a woman's uterus close to the time of ovulation. The procedure is performed by a fertility specialist and usually takes just a few minutes. The sperm used in the IUI can be from the woman's partner or from a donor. The process is less invasive and less expensive than other fertility treatments like in vitro fertilization (IVF). IUI can be used alone or in combination with ovulation induction or other fertility drugs to enhance the chances of pregnancy. The success rate of IUI varies depending on a number of factors such as age and the causes of infertility. However, for many couples struggling with infertility, IUI can provide a safe and effective solution to help them conceive a child.c. In Vitro Fertilisation (IVF):
In vitro fertilization (IVF) is a type of assisted reproductive technology (ART) in which eggs are removed from a woman's ovaries and fertilized with sperm in a laboratory. The resulting embryos are then transferred back into the woman's uterus with the hope of achieving pregnancy. IVF is commonly used for couples facing infertility due to problems with ovulation, damaged or blocked fallopian tubes, or male factor infertility. The process involves several steps, including ovulation induction, egg retrieval, fertilization, embryo culture, and embryo transfer. IVF can be a highly effective treatment for infertility, but it can also be expensive, time- consuming, and physically and emotionally demanding. The success rate of IVF varies depending on factors such as the woman's age, the cause of infertility, and the number of embryos transferred. However, for many couples, IVF provides a path to parenthood and can result in the birth of a healthy baby.d. Intra Cytoplasmic Sperm Injection (ICSI):
Intracytoplasmic sperm injection (ICSI) is a type of assisted reproductive technology (ART) that is often used in conjunction with in vitro fertilization (IVF). In ICSI, a single sperm is directly injected into an egg in order to fertilize it. The procedure is performed in a laboratory by an embryologist and is used for cases of male factor infertility, such as low sperm count or poor sperm motility. ICSI can also be used for couples where previous IVF cycles have failed. The fertilized egg (embryo) is then cultured in the laboratory and, if successful, is transferred back into the woman's uterus. The success rate of ICSI is comparable to that of IVF, but it can be more expensive and time-consuming. However, for many couples facing infertility, ICSI provides a path to parenthood and can result in the birth of a healthy baby.e. Frozen Embryo Transfer (FET):
Frozen Embryo Transfer (FET) is a procedure used in assisted reproductive technology (ART) where previously frozen embryos are thawed and transferred back into a woman's uterus with the goal of achieving pregnancy. FET is often performed after an in vitro fertilization (IVF) cycle, when there are extra embryos remaining that have been frozen and stored. The process of freezing and thawing embryos has become much more successful over the years and has become a commonly used option for couples facing infertility. FET has several benefits, including a lower cost compared to a fresh IVF cycle, the ability to choose the timing of the transfer, and less physical and emotional stress for the woman. The success rate of FET varies depending on factors such as the woman's age and the quality of the embryos. However, for many couples, FET provides a path to parenthood and can result in the birth of a healthy baby.f. Egg Freezing:
Egg freezing, also known as oocyte cryopreservation, is a medical procedure that involves freezing a woman's eggs for future use in assisted reproductive technology (ART) such as in vitro fertilization (IVF). The process involves retrieving a woman's eggs, freezing them, and storing them in a laboratory until they are needed. Egg freezing is often used by women who are not yet ready to have children but want to preserve their fertility for the future. It can also be used for women facing medical conditions or treatments that may negatively impact their fertility, such as cancer or radiation therapy. The success rate of egg freezing, and subsequent fertilization depends on several factors such as the woman's age and the quality of the eggs at the time of retrieval and freezing. However, for many women, egg freezing provides peace of mind and a potential solution for future infertility problems.g. Sperm Freezing:
Sperm freezing also known as sperm cryopreservation, is the process of freezing and storing semen samples for future use in assisted reproductive technology (ART) such as intrauterine insemination (IUI) or in vitro fertilization (IVF). The process involves collecting a semen sample, freezing it, and storing it in a laboratory until it is needed. Sperm freezing is often used by men who want to preserve their fertility for the future, such as those facing medical conditions or treatments that may impact their sperm count or quality, or those who are undergoing vasectomy. It is also commonly used by men who want to donate their sperm for use in donor insemination. The success rate of sperm freezing, and subsequent fertilization depends on several factors such as the quality of the sperm at the time of freezing and the method of ART used. However, for many men, sperm freezing provides peace of mind and a potential solution for future infertility problems. This content is shared with the permission of Dr. Baruah. You may find similar information in health publications.Feeling sick and unsure why? Talk to a doctor online, available 24/7
Consult now
Available 24/7, across Australia.
Feeling sick and unsure why? Talk to a doctor online, available 24/7
Consult now
Available 24/7, across Australia.
Providing consult for
- Cough
- Nausea & vomiting
- Fever
- Hayfever
- Fatigue
- Sore throat
- Acne
- Gout
- Eczema
- Rosacea
- Sunburn
- UTI
- Erectile dysfunction
- Contraception
- Morning sickness
- Morning after pill
- Prostate health
- Anxiety
- Depression
- Stress
- Grief & loss
- Premature ejaculation
- Asthma
- Blood pressure
- Diabetes
- Cholesterol
- Migraines & headaches
- Allergies
- Heartburn & reflux
- Sleep disorder
- Gastro
Related Articles
Disclaimer
This blog is for general informational purposes only and does not indicate that Hola Health provides all treatments or preventive measures mentioned. It is not intended to be a substitute for professional medical advice. Always seek the guidance of your doctor or other qualified health professional with any questions you may have regarding your health or a medical condition. For emergencies please immediately contact 000. Any medical topics discussed are intended to educate, not to imply availability through Hola Health.




